Vascular specialist helps put intravenous lines, patients, and staff in a better place
Howard County General Hospital’s commitment to innovation, collaboration, and safety is in its veins—and those of its patients.
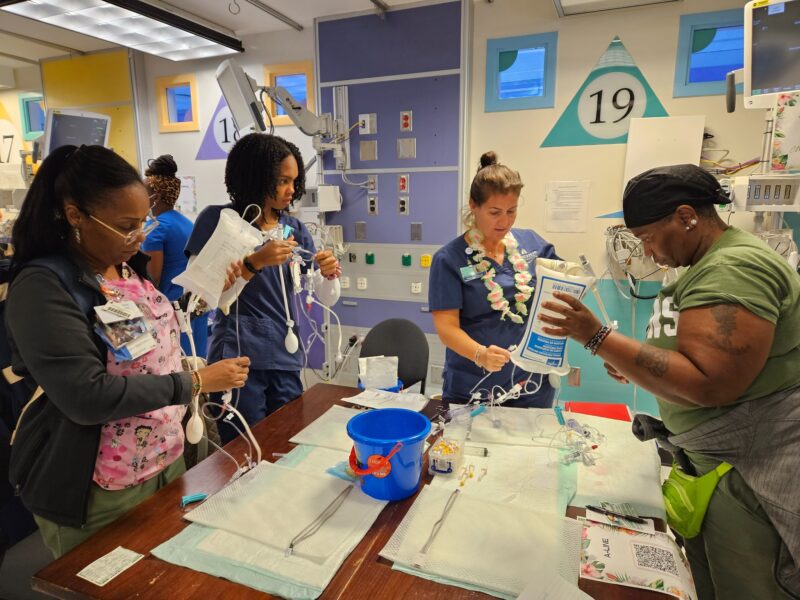
HCGH welcomed a vascular access specialist last year to increase the satisfaction of patients who need intravenous fluids. Loida Lacson, RN, is currently the sole full-time member of the hospital’s vascular access team. HCGH is already evaluating expanding the team since Lacson regularly receives high praise from patients and colleagues alike.
Before she joined HCGH in October 2014, nurses had only two choices for inserting catheters: a typical IV or a peripherally inserted central catheter, known as a PICC line. These are used to reach larger blood vessels in the chest when smaller veins would be damaged by certain medications or when several days of IV access are needed. Because there was no middle option, nurses were forced to use highly invasive PICC lines when regular IVs were inadequate.
Lacson helped institute innovative new options. “PICCs were ordered unnecessarily, like patients getting a PICC for a CT scan,” says Lacson, a certified vascular access nurse. “They got PICCs just for blood draws or a brief hospital stay.”
Instead, Lacson explains, some patients need a midline catheter, which provides a third, often more appropriate method of vascular access. A midline catheter is less invasive than a PICC line and can be used up to six weeks, unlike regular IVs, which must be changed about every four days. Therefore, patients can go home with the treatment.
“We no longer have to say, ‘Oh, we can’t do that, so we’re going to do this,’ ” says Bridget Carver, RN, the hospital’s cardiovascular lab manager. “We have a wider range of tools now.”
Lacson assesses each patient and inserts the appropriate access, starting with the least invasive. Most of the time, she inserts the ultrasound guided peripheral IV—at a 99.9% success rate. (If this is not a good option based on patient condition or the therapy needed, she goes to more invasive lines starting with the midline and using the PICC only if absolutely necessary.) Before the hospital bought the new equipment, nurses had to use a chest X-ray or fluoroscopy to ensure accuracy. “I always hear from patients and patients’ families that they feel less anxious with this bedside procedure,” Lacson says. “It’s quicker, less painful, and there’s less exposure to radiation.”
In fact, everyone is happier. Patients no longer have long waits for their IV or delays in leaving the hospital. Nurses don’t waste time transferring patients to radiology for fluoroscopy-guided PICC lines, and they can use PICC lines sooner after placement. Radiologists rarely have PICC cases in the labs. And Lacson is happy to have eased their load. “I am here with a purpose,” she says, “to protect the patients and help my colleagues.”
Illustration by Leonard Peng